

Published on January 8, 2026 By 800ZED

Adie thought he was just tired. After several sleepless nights and a stressful week, he noticed muscle weakness and soreness in his left shoulder down to his forearm. A pain reliever helped at first, so he brushed it off...no chest pain, no classic “heart attack” drama, so how serious could it be?
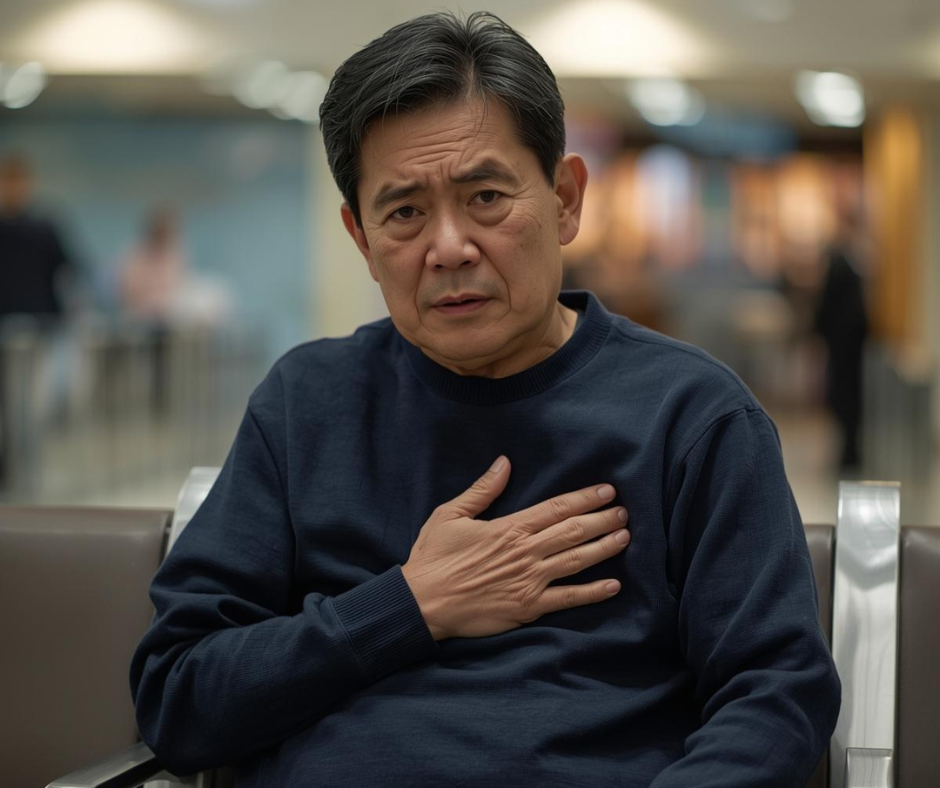 A week later, while walking in the mall, everything changed. He suddenly felt his chest grow heavy, his lips turned pale, and he became short of breath. Pain spread from his jaw to his shoulder and down his left arm. Thinking it might be a tooth problem, he tried to treat it like a dental issue but the pain reliever didn’t work. When he finally went to the emergency medicine team at the hospital, doctors confirmed he was having a myocardial infarction: a heart attack.
A week later, while walking in the mall, everything changed. He suddenly felt his chest grow heavy, his lips turned pale, and he became short of breath. Pain spread from his jaw to his shoulder and down his left arm. Thinking it might be a tooth problem, he tried to treat it like a dental issue but the pain reliever didn’t work. When he finally went to the emergency medicine team at the hospital, doctors confirmed he was having a myocardial infarction: a heart attack.
Stories like this matter because many people still miss early warning signs. And to make things more confusing, heart attacks and strokes are often lumped together as “cardiovascular disease,” even though they affect different parts of the body.
A heart attack (myocardial infarction) happens when blood flow to part of the heart muscle is blocked, usually in the coronary arteries.
A stroke happens when blood flow to part of the brain is blocked (ischemic stroke) or when a blood vessel in the brain bursts (hemorrhagic stroke).
In both cases, cells are starved of oxygen. The longer the blockage lasts, the more tissue dies; heart cells in a heart attack, brain cells in a stroke, so rapid treatment from an emergency medicine team is critical.

Most heart attacks start with a problem in the coronary arteries, the blood vessels that feed the heart muscle. Over time, fatty deposits, cholesterol, calcium, and other substances build up in the artery wall and form plaque; this slow, silent process is called atherosclerosis.
If a plaque ruptures, the body forms a clot to “repair” it, but that clot can fully block the artery, cutting off oxygen and causing a myocardial infarction.
Some heart attacks can occur even without a clear blockage on standard imaging, due to:
Severe spasms of the coronary arteries
Spontaneous tearing in a coronary artery wall
Micro‑vessel or clotting problems
Conditions like myocarditis or stress‑induced cardiomyopathy
That is why a cardiology team looks at symptoms, ECG changes, and blood tests such as troponin, a protein released when heart muscle cells are injured.
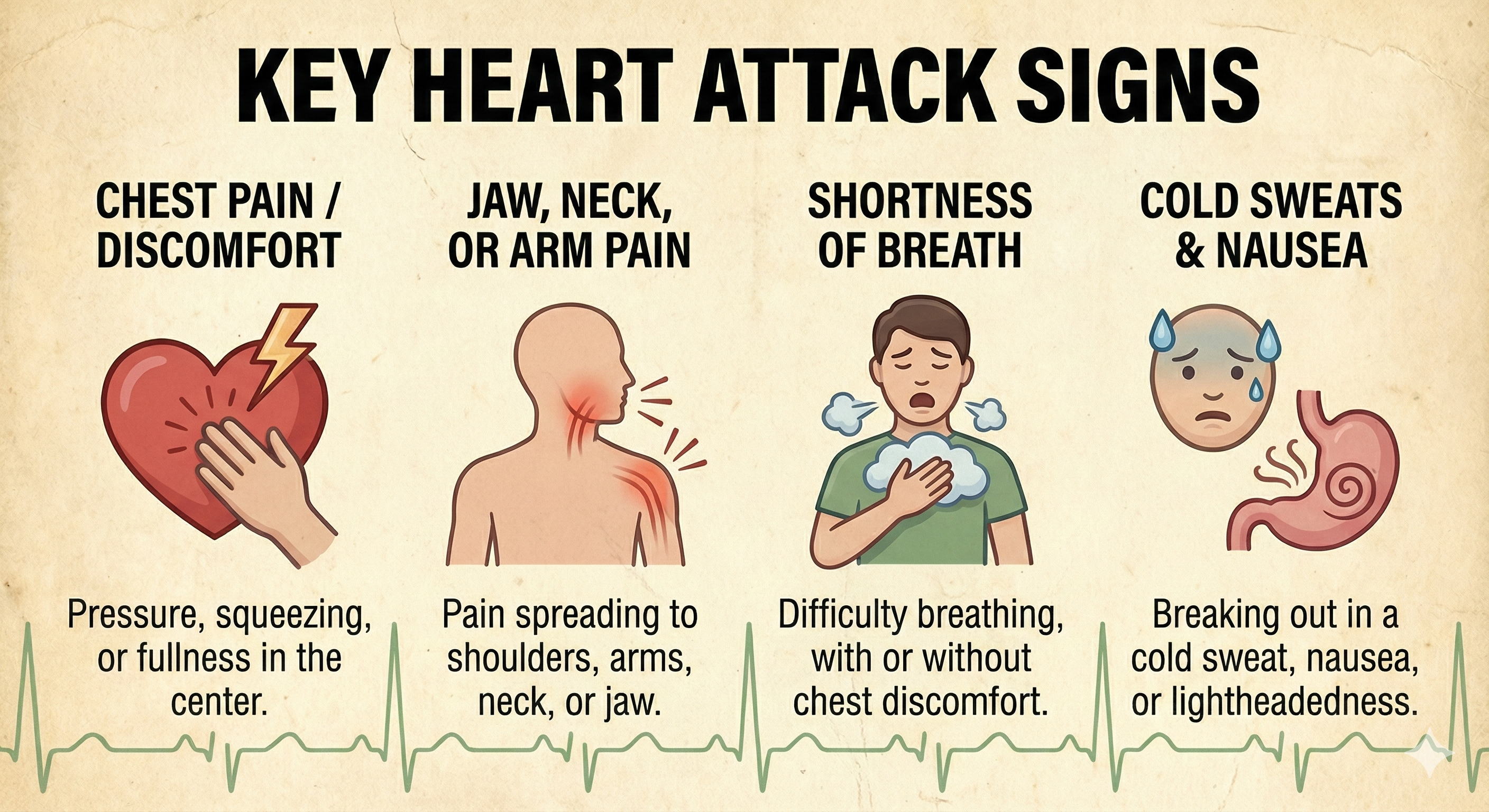
“Classic” heart attack symptoms include:
Chest heaviness, squeezing, or pressure (often in the center or left side)
Pain that may spread to the jaw, neck, back, or left arm
Shortness of breath
Cold sweat, nausea, or sudden lightheadedness
Unusual fatigue or a sense that “something is very wrong”
Not everyone has textbook chest pain. Women, older adults, and people with diabetes may have more subtle symptoms like fatigue, shortness of breath, indigestion‑like discomfort, or back or jaw pain without obvious chest pressure.
Whatever the pattern, new, persistent, or worsening chest discomfort or unexplained upper‑body pain is a reason to seek urgent care from emergency medicine and then follow‑up with cardiology, not just take a pain reliever and wait.
A stroke also involves interrupted blood flow...but this time to the brain. There are two main types:
Ischemic stroke: A blood clot blocks an artery in or leading to the brain (most common).
Hemorrhagic stroke: A blood vessel in the brain ruptures and bleeds, damaging surrounding brain tissue.
Because different parts of the brain control different functions, stroke symptoms depend on which area is affected, but they almost always start suddenly. Brain cells begin to die within minutes, so fast treatment through emergency services is essential.

A quick way to remember stroke warning signs is F.A.S.T.:
F – Face: Sudden drooping or numbness on one side of the face. Ask the person to smile—does one side sag?
A – Arms: Weakness or numbness in one arm or leg on one side of the body. Ask them to raise both arms—does one drift down?
S – Speech: Slurred speech, trouble finding words, or difficulty understanding others.
T – Time: Time to call emergency services immediately. Do not wait “to see if it goes away.”
Other possible stroke symptoms include sudden confusion, trouble walking, loss of balance, severe headache with no clear cause, or sudden vision problems in one or both eyes.
Both are medical emergencies. The goal in both situations is the same: restore blood flow as quickly and safely as possible.
Even though heart attacks and strokes affect different organs, they often share the same underlying risk factors because they begin with long‑term blood‑vessel damage.
Problems like high blood pressure, high LDL cholesterol, smoking, diabetes, obesity, and chronic stress all attack your circulation over time.
High blood pressure injures arteries in the heart and brain, making clots and blockages more likely—this is why regular follow‑up with a hypertension specialist or internal medicine doctor matters.
High LDL cholesterol and smoking speed up plaque build‑up in arteries all over the body, not just around the heart.
Diabetes, central obesity, and inactivity increase inflammation and stiffen blood vessels, raising the risk of both heart attack and stroke.
 Together, these risk factors make arteries narrower, stiffer, and more likely to develop plaque and clots. The same process that blocks a coronary artery and triggers a heart attack can also block an artery leading to the brain and cause a stroke.
Together, these risk factors make arteries narrower, stiffer, and more likely to develop plaque and clots. The same process that blocks a coronary artery and triggers a heart attack can also block an artery leading to the brain and cause a stroke.
The good news: many of these risks improve with early treatment, lifestyle changes, and regular care from internal medicine, cardiology, and hypertension specialists.
For both heart attack and stroke, time is everything.
Seek emergency care immediately if you notice:
Sudden chest pressure, heaviness, or pain that does not go away with rest
Pain that spreads to the jaw, neck, back, or left arm, especially with shortness of breath, sweating, or nausea
Any F.A.S.T. stroke signs: face drooping, arm weakness, speech difficulty, or sudden confusion, vision changes, or severe headache
Do not wait to see if symptoms pass, and do not just take a pain reliever. Call your local emergency number or go to the nearest emergency room so an emergency medicine team can act fast.
Getting treatment within the first few hours can mean the difference between full recovery and permanent disability—or even life and death.
You cannot change your age or family history, but you can greatly lower your risk of both heart attack and stroke by focusing on daily habits and regular check‑ups.
Helpful steps include:
Know your numbers: Have your blood pressure, blood sugar, and cholesterol checked regularly, especially if you are over 40 or have a family history of heart disease or stroke, ideally with an internal medicine or hypertension specialist.
Quit smoking and avoid vaping nicotine: These directly damage blood vessels and speed up plaque build‑up.
Move your body most days of the week: Even 30 minutes of brisk walking on most days improves circulation, blood pressure, and weight control.
Choose heart‑ and brain‑friendly foods: More vegetables, fruits, whole grains, fish, and healthy fats; less processed meat, fast food, and sugary drinks.
Manage stress and sleep: Chronic stress, poor sleep, and burnout raise blood pressure and inflammation over time.
Take medications as prescribed: If your doctor has given you medicine for blood pressure, cholesterol, diabetes, or blood thinners, consistency is crucial to prevent future events that might need cardiology or vascular surgery care.
If you have frequent chest discomfort, unexplained shortness of breath, sudden weakness, or a strong family history of heart disease or stroke, do not wait for an emergency.
heart disease or stroke, do not wait for an emergency.
An 800ZED Internal Medicine, Cardiology, Hypertension, or Thoracic, Cardiac and Vascular Surgery consult—through telemedicine, clinic visit, or home visit can help you:
Review your personal and family risk factors
Interpret your blood pressure, sugar, and cholesterol results
Create a realistic plan to protect both your heart and brain and know when to seek emergency medicine support
Recognizing the difference between a heart attack and a stroke and knowing when to call for help and when to see the right 800ZED specialist can save a life, including your own.
We use cookies to give you the best service on our site. By continuing to use the site you consent to our Privacy Policy
📲 Install 800 ZED App for quick access!
📲 Install 800 ZED App on your iPhone
Tap Share → Add to Home Screen
📲 Install 800 ZED on Firefox
Open menu ☰ → Install
Subscribe our newsletter for latest updates
Get the latest updates, promotions, and news delivered straight to your inbox.